Introduction
To the untrained eye, the symptoms of Chronic Obstructive Pulmonary Disease (COPD) and asthma can appear very similar. Both are chronic respiratory conditions that cause shortness of breath, coughing, and wheezing. However, beneath the surface, they are fundamentally different diseases that require distinct treatment strategies. Misdiagnosing one for the other can lead to ineffective therapy and a worsening of a patient’s condition. This is where a lung function test, specifically spirometry, becomes the single most important diagnostic tool. While a physical exam and patient history can suggest a diagnosis, spirometry provides a definitive, objective answer. This article will walk you through the differences between COPD and asthma and explain how the results of a simple breathing test are the key to telling them apart.
Understanding COPD and Asthma
Before diving into the diagnostic process, it’s important to understand the core differences between these two conditions.
Asthma
Asthma is a chronic inflammatory disease of the airways. It is characterized by reversible episodes of bronchoconstriction. Think of an asthmatic’s airways as “twitchy” or “hyper-responsive.” They are highly sensitive to triggers like allergens (pollen, pet dander), exercise, or cold air. When exposed to a trigger, the muscles around the airways tighten, and the lining swells with inflammation and mucus, causing a temporary but significant narrowing. Because this narrowing is caused by muscle constriction, it can be relaxed with the right medication. [1]
COPD
Chronic Obstructive Pulmonary Disease is a progressive, long-term lung disease that causes irreversible airflow limitation. It is primarily caused by long-term exposure to irritants, most notably cigarette smoke, but also secondhand smoke, air pollution, and occupational dust. COPD is a combination of two primary conditions:
- Chronic Bronchitis: Constant inflammation of the airways, leading to a persistent cough and excess mucus.
- Emphysema: The destruction of the tiny air sacs (alveoli) at the end of the airways.
Unlike asthma, the damage in COPD is permanent. The airway walls are no longer just tight; they are physically scarred and destroyed, making it impossible for the airway to open fully again. [2]
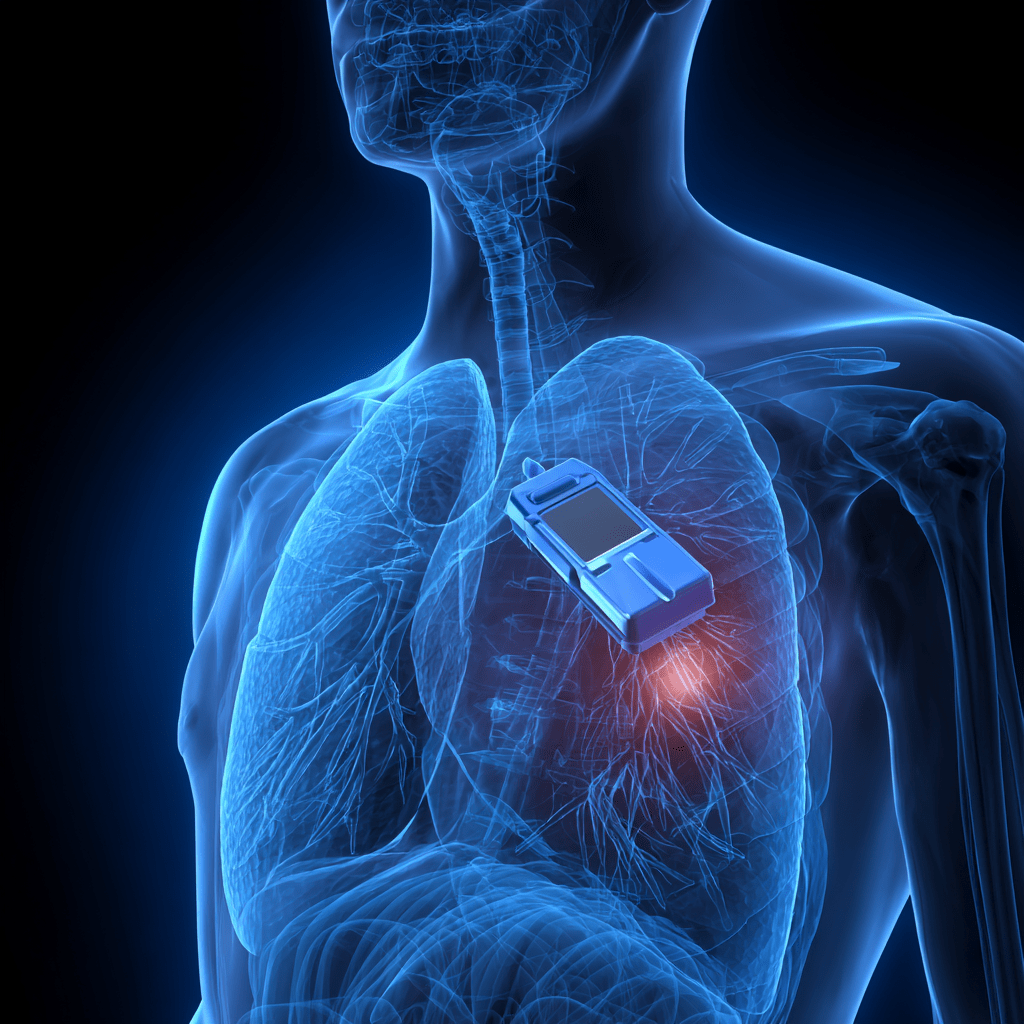
What is Spirometry?
Spirometry is the most common lung function test used to diagnose and monitor lung conditions. It is a simple, non-invasive test where the patient breathes into a device called a spirometer. The machine measures two key values:
- Forced Vital Capacity (FVC): The total amount of air you can forcefully exhale after taking the deepest breath possible.
- Forced Expiratory Volume in 1 second (FEV1): The amount of air you can forcefully exhale in the first second of the test.
The most critical number for diagnosing an obstructive lung disease is the FEV1/FVC ratio. A low ratio indicates that there is a problem with airflow out of the lungs. [3]
Differentiating with Reversibility
While a low FEV1/FVC ratio can confirm that a patient has an obstructive lung disease, it cannot tell you if it is asthma or COPD. This is where the bronchodilator challenge comes in. This is the single most important step in the diagnostic process.
Here’s how it works:
- Baseline Test: The patient performs a standard spirometry test to get their initial FEV1 and FVC values.
- Bronchodilator Administration: The patient is then given a dose of a short-acting bronchodilator, such as albuterol, via an inhaler or nebulizer.
- Post-Test: After a waiting period (typically 10-15 minutes), the patient repeats the spirometry test.
The results of this second test provide the definitive answer to whether the airflow obstruction is reversible.
- The Asthma Response (Reversible Airflow Limitation): For a person with asthma, the bronchodilator will relax the muscles around the airways. When the patient performs the second spirometry test, the FEV1 and FVC will show a significant improvement (a clinically significant increase, typically >12% and >200 mL). This improvement proves that the obstruction was temporary and caused by muscle constriction, not permanent damage. This is the hallmark of asthma. [4]
- The COPD Response (Irreversible Airflow Limitation): For a person with COPD, the bronchodilator will have little to no effect. The FEV1 will not significantly improve because the airway obstruction is caused by irreversible damage to the airways and air sacs. You cannot relax tissue that has been destroyed. This lack of reversibility is the defining characteristic of COPD. [5]
The Impact of the Diagnosis
This diagnostic distinction is not just an academic exercise; it is crucial for a patient’s health. The treatment for each condition is different.
- Asthma Treatment: The focus is on quick-relief inhalers to relax muscles during an attack and long-term control medications (most commonly inhaled corticosteroids) to reduce the underlying airway inflammation and prevent future attacks.
- COPD Treatment: The focus is on long-acting bronchodilators to keep the airways as open as possible, supplemental oxygen therapy in advanced stages, and most importantly, lifestyle changes like smoking cessation to prevent further disease progression. [6]
Because asthma is a highly manageable condition with a good long-term prognosis and COPD is a progressive, worsening disease, an accurate diagnosis is the first and most critical step in ensuring a patient receives the correct care. Spirometry, especially with the bronchodilator challenge, provides the unambiguous data needed to make that correct diagnosis and improve a patient’s long-term quality of life. [7]
