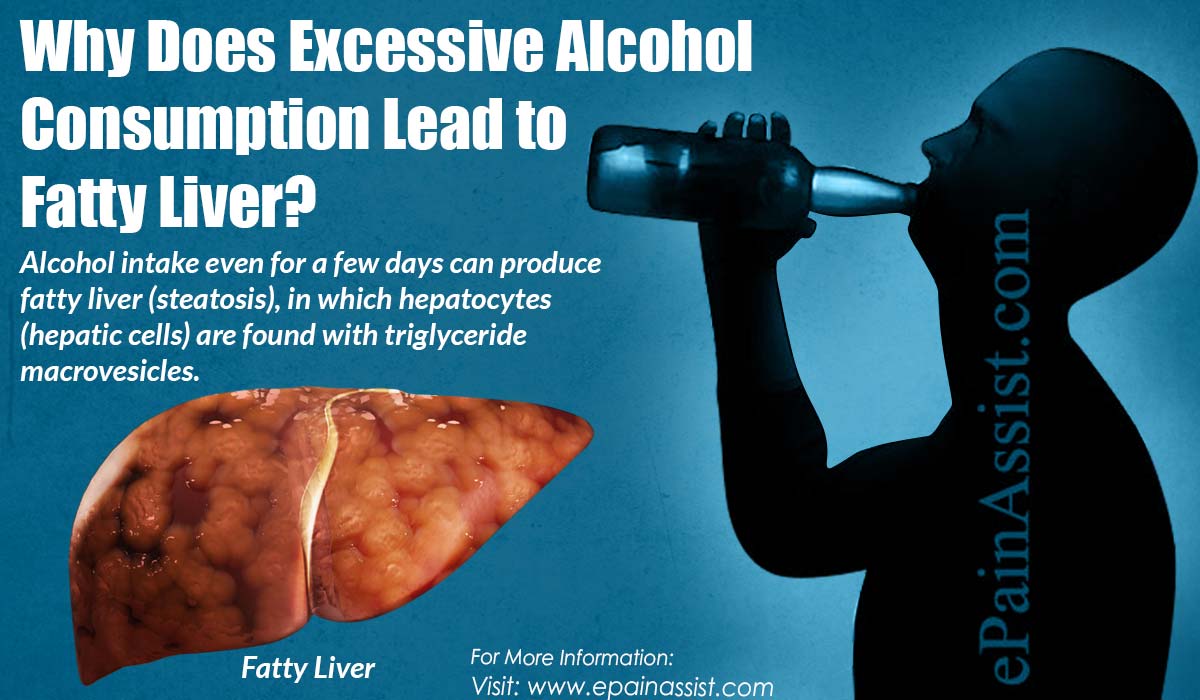
Why Does Excessive Alcohol Consumption Lead to Fatty Liver?
Alcohol intake even for a few days can produce fatty liver (steatosis), in which hepatocytes (hepatic cells) are found with triglyceride macrovesicles.
Although alcoholic fatty liver improves with abstinence, steatosis predisposes individuals who continue to drink to liver fibrosis and cirrhosis. The risk of cirrhosis increases proportionally with the intake of 30 grams of alcohol or more per day. The highest risk is associated with the consumption of 120 grams of alcohol or more per day. There are other factors that accelerate the progression of alcoholic liver disease, such as female sex, genetic characteristics, overweight, and infection with hepatitis B and C viruses, tobacco, among others.
Hepatic alcoholic disease presents a broad spectrum ranging from simple fatty liver to the most severe forms of liver disease, including alcoholic hepatitis, cirrhosis and hepatocellular carcinoma.
These are different stages that can be simultaneously present in the same individual.
In addition, they may be associated with various histological changes, which have different degrees of specificity for alcoholic liver disease (ALD), including the presence of Mallory bodies, megamitochondria, perivenular and/or perisinusoidal fibrosis, and sclerosing hyaline necrosis. Fatty liver (an early response to alcohol consumption) develops in most drinkers; mild steatosis is in the hepatocytes of zone 3 (perivenular), it can also affect zone 2 and even hepatocytes in zone 1 (periportal) when the liver injury is more severe. Only about 30% of drinkers develop more serious forms of ALD, such as fibrosis and cirrhosis.
The simple fatty liver is usually asymptomatic and self-limited and can be completely reversible with abstinence of 4 to 6 weeks. However, some studies suggest that progression to fibrosis ranges from 20 to 40%, and in these cases, between 8 and 20% may progress to cirrhosis despite being in abstinence.
Fibrosis begins in the perivenular area and is influenced by the amount of ingested alcohol. Perivenular fibrosis occurs in 40 to 60% of patients who ingest more than 40 to 80 grams per day for an average of twenty-five years. Perivenular sclerosis has been identified as an important and independent risk factor for the progression of liver injury to fibrosis or cirrhosis, which may be micronodular, but can sometimes be mixed micronodular and macronodular.
A subgroup of patients with ALD will develop severe alcoholic hepatitis (AH), whose prognosis is substantially worse in the short term. AH ranges from mild to severe injuries and life-threatening injuries, and usually presents acutely on chronic liver damage. It’s true prevalence is unknown, but histological studies of patients with ALD suggest that AH may be present in 10 to 35% of hospitalized alcoholic patients.
Cirrhosis develops up to 50% in these cases. The likelihood of AH progressing is greater among those who continue to abuse alcohol. The alcohol abstinence in small series does not guarantee complete recovery. Only 27% of the patients with abstinence had a histological normalization, while 18% progressed to cirrhosis; the rest of the patients had persistent HA when it was followed for more than 18 months.
Risk Factors
The likelihood of developing progressive liver disease induced by alcohol is not completely dose-dependent; this occurs in only a subset of patients.
There are some identified risk factors that influence the risk of development and the progression of liver disease.
The amount of ingested alcohol (regardless of the type of used alcoholic beverage) is the most important risk factor for the development of ALD. There is a significant correlation between per capita consumption and the prevalence of cirrhosis. The fact that only about 35% of excessive drinkers develop severe ALD indicates that they are involved other risk factors.
Conclusion
Alcohol abstinence is the most important therapeutic intervention in the ALD. It has been observed that abstinence improves the prognosis and histological findings of liver damage, decreases steatosis (accumulation of fat in the liver), portal pressure and progression to cirrhosis. In addition, it improves the survival in all stages of ALD.
Also Read:
