Continuous and prolonged pressure to the skin causes injury to the skin and its underlying tissue resulting in Decubitus Ulcer or Pressure Ulcer or Bedsores. Decubitus ulcers commonly develop on the skin, which covers the bony parts of the body, such as ankles, heels, hips and tailbone. Individuals who are invalids and are confined to bed or wheelchair and who cannot move or change their position are more likely to develop bedsores decubitus ulcers. Decubitus ulcers tend to develop quickly and they can be quite difficult to treat.
Treatment comprises of cleaning the ulcers, applying dressings, wound debridement and surgery if needed.
Causes of Decubitus Ulcer or Pressure Ulcer or Bedsores
Decubitus Ulcer or Pressure Ulcer or Bedsores occur as a result of continuous pressure against the skin, which restricts the blood flow to the skin and adjacent tissues. There are 3 main contributing factors which limits a person’s mobility and makes the skin more prone to damage and ultimately developing decubitus ulcers. They are:
- Continuous pressure where the skin and the underlying tissues is trapped or caught between the bone and other surfaces, like a bed or a wheelchair. This restricts the blood flow to the tissues resulting in damage to the skin cells and tissue. Areas which aren’t well padded with either fat or muscle are more prone to such kind of pressure. These areas include: Bony surfaces, such as skin over the bone, spine, joint-pain/shoulder-pain/shoulder-blade-pain, shoulder blades, tailbone, hips, elbows and heels.
- Friction is another contributing factor and this may occur if the skin is pulled across a surface such as when the patient is changing his/her position or if some else moves him/her. A moist skin increases the friction even more. Friction makes the already fragile skin more predisposed towards the breakage and injury.
- Shear occurs when two surfaces are moved in the opposite directions, such as when the hospital bed is raised at the head and the patient slides down in the bed. This results in the tailbone moving down, but the skin over the tailbone remaining in place, causing it to pull in opposite directions and leading to injury of the tissue and blood vessels. This in turn makes this area more prone to damage from prolonged pressure.
Risk Factors for Decubitus Ulcer or Pressure Ulcer or Bedsores
Individuals who are confined to one place and cannot move or change their position are at a great risk for developing Decubitus Ulcer or Pressure Ulcer or Bedsores. The reason for this immobility includes:
- Medical conditions where you cannot move, such as paralysis.
- Weak or poor health.
- Any illness or injury which requires bed rest or the use of a wheelchair.
- Recovering after a surgical procedure.
- Coma or sedation.
- Older or aged individuals are more prone to developing decubitus ulcers, as their skin is more thin, dry and fragile with decreased elasticity. The production of new skin cells is also less in older individuals, which makes their skin more vulnerable to damage.
- Injury to the spinal cord or neurological disorders decreases a person’s sensory perception and this causes loss of sensation due to which the patient is not able to feel any pain or discomfort from the bedsores and thus doesn’t feel the need to change his/her position.
- Loss of weight, muscle atrophy and wasting due to prolonged illnesses results in loss of muscle and fat due to which there is decreased cushioning between bones and other surfaces, like wheelchair or a bed.
- Skin with excess moisture or dryness is more prone to injury and increased friction between the skin and other surfaces.
- Individuals with poor diet, nutrition and hydration will have an unhealthy skin and tissues, which are more prone to damage and breakdown.
- Medical conditions, such as diabetes, vascular disease etc. affects the blood circulation and increases the risk of damage to the skin and tissues.
- Individuals with frequent muscle spasms are at an increased risk of decubitus ulcers due to repeated friction.
- Bacteria due to bowel/bladder incontinence can result in severe local infections, which can have an effect on the entire body.
- Individuals with limited or decreased mental alertness due to any trauma, disease, or medications cannot properly take care of their decubitus ulcers.
- Smoking also restricts the blood flow, which in turn decreases the oxygen content in the blood. This will result in more severe wounds, which heal slowly.
Signs and Symptoms of Decubitus Ulcer or Pressure Ulcer or Bedsores
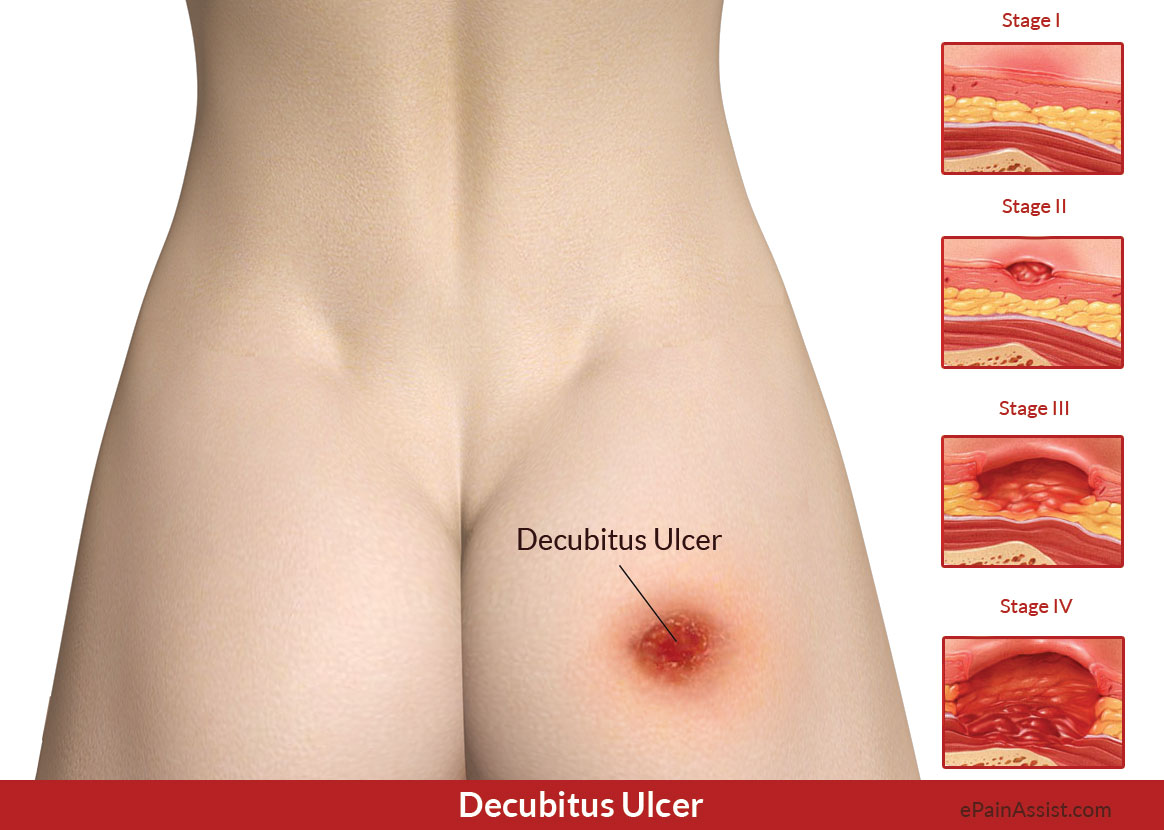
Stage I of Decubitus Ulcer or Pressure Ulcer or Bedsores Has The Following Characteristics:
- There is no tear or beak in the skin.
- Individuals with light or fair skin will have redness to the skin and it doesn’t blanch or lighten upon light pressure.
- Individuals with darker skin may have discoloration with again absence of blanching upon touch.
- The area is painful, tender, soft or firm; cool or warm to touch when compared to the surrounding skin.
Stage II of Decubitus Ulcer or Pressure Ulcer or Bedsores Has The Following Characteristics:
- Damage or absence of the epidermis (outer layer) and some part of the dermis (underlying skin layer).
- The sore appears to be shallow and pinkish or red in color.
- The sore appears as a fluid-filled or a ruptured blister.
Stage III of Decubitus Ulcer or Pressure Ulcer or Bedsores Has The Following Characteristics:
- The ulcer is very deep.
- Underlying fat can be seen due to the skin loss.
- The ulcer has a crater-like appearance.
- There may be some yellowish colored dead tissue at the base of the wound.
- The damage can be beyond the primary wound and also underneath the layers of healthy skin.
Stage IV of Decubitus Ulcer or Pressure Ulcer or Bedsores Has The Following Characteristics:
- There is extreme tissue loss at this stage.
- The wound is deep, exposing the underlying muscle, tendons or bone.
- Presence of yellowish or dark colored, crusty dead tissue at the base of the wound.
- The damage is deep and can extend past the primary wound and under the healthy skin.
Seek immediate medical attention if there are any signs of infection like drainage, fever, foul odor, increase in redness and heat from the ulcer and its surrounding skin.
Investigations for Decubitus Ulcer or Pressure Ulcer or Bedsores
- Blood tests to check for other medical conditions.
- Tissue cultures are done to find out if there is any bacterial or fungal infection in the wound.
- Tissue cultures are also done to test for any cancerous tissue if the wound is chronic and is not healing.
Treatment for Decubitus Ulcer or Pressure Ulcer or Bedsores
Conservative treatment is sufficient for stage I and II decubitus ulcers and they commonly heal within some weeks to months.
Stage III and IV decubitus ulcers are quite difficult to treat. Treatment comprises of reducing the pressure on the regions of the sores and this is done by:
- Repositioning the patient regularly by shifting the patient’s weight every 10-15 minutes. If the patient is confined to a bed, then he/she needs a position change at least every two hours.
- Using supportive surfaces, such as special cushions, mattress which will help the patient to lie in suitable position, which will help in relieving the pressure on the sores and also in protecting the fragile skin. A cushion can be used if the patient is confined to a wheelchair.
- Cleaning the wounds is important. The wounds are cleaned to help prevent infection. For stage I ulcers, the wounds are gently washed with a mild soap and water and are gently patted dry. If the sores are open or have a broken skin, then they are cleaned with saline water before the dressing change.
- Applying dressings helps in promoting the healing process. Dressings keep the wound moist and create a barrier against infection along with keeping the surrounding region dry. Dressings can be done with gauzes, films, foams, gels and treated coverings. A combination of these dressings can also be used.
The damaged/infected tissue needs to be removed or debrided to allow proper healing. Depending on the stage of the ulcer, patient’s general health, the goal of treatment, debridement is done in the following ways:
- Mechanical debridement helps in loosening and removing the debris in the wound. This is accomplished using a pressurized irrigation device, specialized dressings or low-frequency mist ultrasound.
- Surgical debridement comprises of excising the dead tissue.
- Enzymatic debridement comprises of application of chemical enzymes and special dressings to breakdown the necrotic tissue.
- Autolytic debridement boosts the body’s natural process, which uses enzymes to breakdown the necrotic tissue. This method can be done on smaller wounds which are not infected. This method also involves the use of special dressings in order to keep the wound clean and moist.
Medications Used for Decubitus Ulcer or Pressure Ulcer or Bedsores Include:
- Pain killers or NSAIDs (Nonsteroidal Anti-Inflammatory Drugs), such as ibuprofen and naproxen, help with the pain and inflammation. Topical pain medications are also beneficial during the process of debridement and while changing the dressings.
- Topical or oral antibiotics are prescribed if the sores or ulcers are infected and are not responding to other treatments.
- Muscle relaxants, such as diazepam, tizanidine and baclofen, are prescribed if the patient has muscle spasm, as muscle spasms cause increase in friction.
- Bladder or bowel incontinence causes increased bacteria and moisture on the skin which in turn increases the risk of infection. It is important to manage incontinence properly by a proper scheduled help with frequent diaper changes, urinating and application of protective lotions.
- A healthy diet consisting of high-protein, vitamins and minerals is a must to promote healing. Dietary supplements, such as zinc and vitamin C, are also prescribed.
- Vacuum-Assisted Closure (VAC)/ Negative Pressure Therapy comprises of using a suction device to clean the wound. It can also aid in healing of the sores.
Surgery for Decubitus Ulcer or Pressure Ulcer or Bedsores
If the Decubitus Ulcer or Pressure Ulcer or Bedsores does not respond to the above measures, then surgery may be required. The aim of surgery is improvement in the appearance of the ulcer and hygiene, preventing/ treating the infection, cutting down the loss of fluid through the wound and reducing the risk of cancer.
The type of surgical procedure done depends on the location of the ulcer and formation of scar tissue from any previous surgery. The common method in surgical repair of decubitus ulcer is covering the wound and cushioning the affected bone (flap reconstruction) with a pad of your muscle, skin or other tissue.
Also Read: